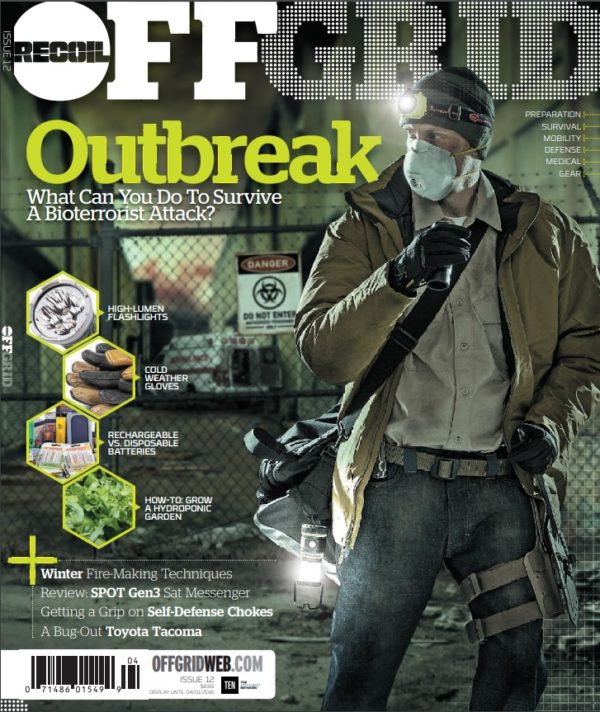
RECOIL OFFGRID Preparation Flu Pandemics of the Past 110 Years
In This Article
This article was originally published in Issue 2 of our magazine.
1918-1919
20-50 million deaths
One of the deadliest outbreaks, ever — not just in terms of the number killed, but also in how quickly they were killed. It is estimated that one third of the world’s population was infected, resulting in 20 to 50 million deaths (some researchers peg the number closer to 100 million). Not only that, but the virus killed mostly healthy young adults instead of the old and weak, who are usually more at risk with influenzas. The death toll in the U.S. was roughly 675,000. Just as quickly as it laid waste to the globe, it disappeared. Its exact origin remains unknown and a topic of debate.
1957-1958
1-4 million deaths
First identified in China, this influenza A virus killed an estimated 1 to 4 million people, including about 70,000 in the U.S. It was relatively less lethal and mostly affected children and the elderly, with an estimated fatality rate of less than 0.2 percent. Vaccines were developed within about three months, but took some time longer to manufacture in quantity. Two waves of infections hit the U.S., a reminder that even when things seem to be getting better during a pandemic, another surge might hit.
1968-1969
1-4 million deaths
Originating from Hong Kong, another influenza A virus spread across the world. An estimated 1 to 4 million people died, about 34,000 of whom were in the U.S. As with the previous Asian Flu pandemic, the fatality rate was also relatively low, at less than 0.2 percent. Additionally, better medical care and antibiotics that helped fight secondary bacterial infections were able to soften the impact.
2009
150k-600k deaths
A new strain of the H1N1 influenza virus from the early 1900s returned in 2009, resulting in an estimated 150,000 to 600,000 dead with a 0.03-percent fatality rate. It hit young people, in particular (5 to 30 years old) with even the very healthy potentially developing pneumonia or acute respiratory distress syndrome. The CDC estimates that in the U.S., about 9,000 to 18,000 people died, out of 43 to 89 million who had H1N1. The virus originated in Mexico, apparently from a combination of pig, bird, swine, and human flu viruses. But, despite the “swine flu” moniker, it had nothing to do with eating pork.
SARS (Severe Acute Respiratory Syndrome)
2002-2003
In 2002 to 2003, severe acute respiratory syndrome (SARS) hit Asia and was a huge scare. Caused by a coronavirus, it resulted in life-threatening atypical pneumonia and respiratory distress. SARS is believed to be transmitted by human-to-human contact, and a quick response by governments, agencies, and citizens helped stop it from spreading and becoming a pandemic. Still, the WHO estimated a 10-percent mortality rate among those who were infected, nearly 800 out of 8,100 across almost 30 countries. Another type of coronavirus, known as the Middle East Respiratory Syndrome coronavirus (MERS-CoV), appeared in Saudi Arabia in 2012. So far, it has remained relatively contained to the Middle East and has not proven to spread rapidly, but it is being closely monitored.
Bird Flu (H5N1)
mid-2000s
You may also remember the Avian Flu (or Bird Flu) from the mid-2000s. This strain of avian influenza (H5N1) was detected in birds, and cases were confirmed in countries across Asia and Europe. It is not considered a pandemic because it lacked means of efficient human-to-human transmission, and total reported cases are relatively low (641 as of October 2013). However, the H5N1 virus is believed to be highly lethal (nearly 60 percent, according to WHO estimates), and if it eventually mutates sufficiently to allow airborne transmission between mammals, it would be extremely dangerous and could quickly rise to pandemic levels. As a result of this looming threat — considered by many to the largest as of today — research and preparation continues in hopes of keeping up with the mutations. Still, keep in mind that it could take several months for production of a new vaccine just to ramp up, much less reach such volumes that they could be widely distributed around the world. And if that wasn’t enough, new variants continue to appear, such as the H7N9 virus that emerged in China in 2013 (as of press date, H7N9 had not yet shown to be transmitted effectively between humans).
Smallpox isn't a form of flu, but there's still much we can learn from this devastating disease. It is caused by the Variola virus, spread by human-to-human contact (e.g. from coughing or exposure to smallpox scabs or contaminated clothing). Initial symptoms typically include fever, vomiting, fatigue, and aches, followed by the infamous rash and bumps spreading from the face to arms and legs. An ancient disease at least 3,000 years old, smallpox killed an estimated 300 to 500 million people in just the 20th century, and it had an estimated mortality rate (depending on who you ask) of 30 to 40 percent among those infected. At least it was a purely human disease, so it could not be transmitted via other means like the bubonic plague.
It is also the only human disease that was defeated by a massive global vaccination campaign. This cross-border achievement, accomplished through cooperation among many nations, is heralded as one of the great triumphs of medical science.
The smallpox vaccine that was developed, comprised of live vaccinia virus, was very effective, but had potentially severe and even fatal complications. Live animals and non-sterile conditions were used to manufacture the vaccine, which would not cut it for current standards. Routine smallpox vaccinations have not been administered for decades. Even if you were vaccinated as a kid, the vaccine requires periodic booster doses to maintain full effectiveness. So the only people walking the streets today truly protected against smallpox are those who already had the disease and survived.
Once smallpox was declared eradicated in 1980, all known stocks of the smallpox Variola virus in laboratories around the world were destroyed or transferred to high-security facilities in the United States and Russia. These are the only official locations that maintain a supply of infectious Variola virus, and research utilizing these samples is tightly restricted and monitored. The World Health Organization and many scientists have urged that the remaining virus stocks be destroyed once and for all, but the U.S. and Russia have resisted, citing research needs.
So, does that give you the warm fuzzies? Yeah, that’s what we thought. So what can you do about it? Follow the same recommendations in the main article, and take some comfort in the fact that smallpox can only be transmitted by person-to-person contact.
These infectious diseases are viruses, so you can’t stock up on antibiotics or other drugs to combat them. You can’t protect against a virus that doesn’t yet exist. However, there are some things you can do to try to stack the odds in your favor:
Maintain your physical condition. Better yet, improve it — exercise and eat healthy. The stronger and healthier you are, the stronger your natural immune system. Keep up to date on your flu shots.
Practice good hygiene. You don’t have to act like Howie Mandel, but wash your hands frequently with soap and water (or alcohol-based hand sanitizer), especially after coughing or sneezing, contact with other people, or touching potentially contaminated surfaces. Cover your coughs and sneezes, and avoid the same from others. Properly dispose of tissues and wash your hands afterward. Avoid touching your eyes, nose, and mouth. For those who hunt or have regular contact with animals, take precautions whenever possible to limit exposure to wild animal blood and bodily fluids, especially if you have any injuries, cuts, or scratches on your hands or arms.
Work to increase your self-sufficiency and preparedness. The more prepared you are with food, supplies, water, and so forth, the better you will be able to wait out quarantines, subsist, and survive during the tough times that may come during a serious and wide-spread pandemic. Try to keep cash and barter goods on hand, since financial services may be disrupted. If you require medications, be sure to keep sufficient stock.
Develop contingency and communication plans for your family. Plan ahead for how to keep in touch, who is responsible for what, and how to corral all your family members.
Distance yourself socially. This is a tough one given the realities of day-to-day life, but avoiding crowds and reducing travel will help decrease your risk of exposure. Try to keep at least a yard away from people who are showing symptoms of influenza-like illness, such as coughing or sneezing.
Keep up to date. Before planning travel, check the latest reports of disease outbreaks: For the U.S., http://www.cdc.gov/flu/weekly/fluactivitysurv.htm, and internationally, http://www.who.int/csr/don/en/index.html.
Stock up on N95 respirators. NIOSH-certified N95 respirators or medical masks can help reduce potential exposure, though by no means can you rely on them to fully protect you.
Avoid urban areas. If possible, residing in areas with a lower population density will reduce your risk to some extent. However, note that in this day and age, even people in rural areas may also travel frequently. You also need to balance population density against having access to quality health care.
It would seem that living like a reclusive hermit might be the safest course of action, but we also can’t live our lives completely in fear. So be smart, stay informed, and be prepared.
Sources
Although it falls under a different classification than the forms of influenza discussed in this article, the 2019 novel Coronavirus (also known as COVID-19) is rapidly developing into a large-scale pandemic. For more information on Coronavirus symptoms, detection, treatment, and prevention, refer to our recent article, Coronavirus: How Concerned Should We Be? by Dr. David Miller.
 STAY SAFE: Download a Free copy of the OFFGRID Outbreak Issue
STAY SAFE: Download a Free copy of the OFFGRID Outbreak Issue
No Comments