RECOIL OFFGRID Survival First Aid in the Field: Become Your Own First Responder
In This Article
It was a spring-like day in early March when I met Nick Gaines. He was our instructor for Prolonged Field Care (PFC), which I would endure over the following 48 hours. Gaines was a former 18D and Special Operations Forces Austere Course (SOFAC) instructor. He currently works as a flight medic in eastern Texas. To our knowledge, this was the first time a PFC course was offered to a civilian cadre over a weekend anywhere in the country. The only prerequisite for the class was that you had to have taken Tactical Combat Casualty Care (TCCC) in the past. Eager students ranged from everyday people to paramedics, law enforcement officers, nurses, and myself. On day one, we reviewed the 75-page guidelines most recently released in December 2021. Day two was a hands-on practical scenario.
Above: Nick Gaines sharing his expertise.
Where TCCC focuses on the immediate care of the casualty, PFC focuses on what happens after stabilization of the life-threatening injury and evacuation to higher care. Transportation of the casualty to definitive care could be hours or even days. An example would be something like this: A mass casualty has occurred. At the scene, the triage would occur, and MARCH protocol would be initiated. A Casualty Collection Point (CCP) would then receive the casualties before transport to the Field Hospital (FH). Once at the FH, the casualty is continually assessed and treated accordingly. Any casualty who needs further treatment is then evacuated to definitive care.
Above: Our field hospital.
The daunting task of whittling down 75 pages of PFC guidelines (www.prolongedfieldcare.org) to an eight-hour course was a challenge that Gaines handled well. An initial caveat that he emphasized was this: “Everyone is expected to participate in their own survival.” With that, he had a captive audience eager to learn more about improving their odds in the austere setting.
After the opening remarks, we started with a brief review of TCCC concepts. Gaines reiterated throughout the day that if you are in a mass-casualty setting and don’t know what to do, go back to the MARCH algorithm. As a quick reminder, the MARCH acronym stands for Massive hemorrhage, Airway, Respiration, Circulation, and Head injury. In PFC, MARCH was expanded to MARCH PAWS L. This added communication as a second “C” in MARCH and continued with Pain, Allergies, Wounds, and Logistics. Once the initial triage was performed, it was necessary to hand the patient off to the next level of care in an efficient manner. We were given the MISTE acronym, which stands for Mechanism of Injury, Injury/Illness type, Signs and Symptoms, Treatments, and ETA to the next level of care. This was one area that many of us took shortcuts on, erroneously, on day two during the scenario.
Above: Field triage of myocardial infarction.
We next reviewed the 10 PFC tasks. The PFC working group developed these to establish a minimum, better, and best practice for PFC of the casualty. For simplicity’s sake, I will list the tasks, and you can read further in the guidelines that I have provided in the link above. The first task is to (1) monitor the casualty to create a useful trend in vitals. Next, (2) resuscitate using blood products if needed. (3) Ventilate and/or oxygenate the patient. (4) Control the airway. (5) Use a sedation or pain control protocol that allows the provider to perform all tasks. (6) Perform a physical exam and any diagnostic measures. (7) Provide nursing care or comfort measures. (8) Perform surgical procedures (e.g., chest tube, cricothyrotomy). (9) Perform a telemedicine consult if needed, and lastly, (10) prepare the patient for transport. The students in the class picked up on many of these tasks, given the brief overview in such a compressed class.
Next, Gaines recognized the daze of the postprandial hypersomnolence that followed lunch. He decided to give us a tour of his truck medic bag and emphasized having items that had multiple uses. He suggested that it wouldn’t be possible to lift the medic’s bag if we tried to plan for every medical emergency we encountered. As it took about half an hour to review the contents of his bag, there wasn’t a space that wasn’t utilized in the bag. Admittedly, my bag isn’t as sexy as his, but you can see mine in Bag Drop of RECOIL OFFGRID Issue 51.
Above: Awaiting transport to Casualty Collection Point.
For the last bit of didactics, we discussed the ramifications and reasoning of tourniquet conversion. The goal of TQ conversion is to move toward a hemostatic agent or a pressure dressing. This can safely be done in the 30- to 120-minute window as long as the bleeding has stopped. The window of two to six hours is also considered safe but not ideal. After six hours, it’s not recommended to convert a TQ unless the casualty is in a definitive care location. The risk of tissue damage, kidney problems, and elevated potassium are problems that could occur after the TQ has been on for greater than six hours.
Day one ended with preparation for the day two scenario. We identified the strengths of the participants and placed them in roles to carry out the following day. We took about 90 minutes to organize during this portion of the class.
Above: SAR assessing the casualty.
We started the morning with a one-hour review of the previous day’s didactic session. We then continued to break down our group into their definitive roles. Overall, there were 24 people in the class. We had an additional 12 casualties for the scenario. The breakdown of our roles for the scenario was as follows: Security (two), search and rescue (two), triage (five), FH (four), transport team (three), resources manager (one), operations manager (one), communications manager (one), medical director (one), logistic coordinator (one), dispatch (one), and incident commander (one). We were given two hours to ready resources such as medical kits, litters, and logistics.
Above: Security taking charge of motor vehicle accident.
As the scenario started, security (two people), SAR team (two people), triage team (five people), comms manager, transport teams (two), and logistics coordinator traveled from FH to CCP. SAR went from the CCP to locate the incident. Once they identified the scene, they radioed for triage and transport to mobilize to the scene. SAR performed the initial TCCC/MARCH assessment. Triage arrived on the scene and started secondary assessments with essential documentation. Casualties were then prioritized and transported to the CCP, which was approximately 500 yards from the incident.
Once at the CCP, Triage performed their assessment and documentation to prepare for transport to FH. Transport took 13 minutes from the CCP to the FH. We used one vehicle for transportation from the incident scene to the CCP and one for transport from the CCP to the FH. Later in the scenario, we used other vehicles to transport casualties to speed up the scenario. Once at FH, four people were serving as nurses. We established a 12-bed FH with one charge nurse and three circulating nurses. The total time of the scenario went from 1,000 to 1,515 hours with no stop for food. The after-action review/debriefing lasted 45 minutes.
Above: Triage team assessing casualties.
There was a consensus that it was a successful learning experience for everyone involved. We proved that you could teach civilians with varying degrees of medical skills the basics of PFC. The exercise was complete chaos for five hours, but everyone did a fantastic job handling their role. The casualties were only given a few items to incorporate into their role play to keep it simple. They did an amazing job as well. We used Zello for our communications during the exercise, which worked out reasonably well. There were lapses in communicating information throughout the exercise, but given the chaos and inexperience of the students, I thought they did an excellent job. The transportation logistics were also a bit of a bottleneck at the scene and CCP. Had there been more participants, this would’ve been the area to bolster aid.
In summary, this was a successful exercise in PFC for the civilian population. During the scenario, everyone was actively involved, and nobody had any downtime during the event. Gaines did an exceptional job presenting the information, and we were pleased with how everything turned out. Everyone, including me, came away with more knowledge to add to their skill set.
Above: Transport team loads casualty.
David L. Miller, DO, FACOI, is an internist in private practice for 20 years. His experiences away from the office have included time as a fight doctor in regional MMA events and as a team physician for 10 years at a midmajor university in the Midwest. Currently, he serves as the lead medical instructor for the Civilian Crisis Response team based out of Indianapolis.
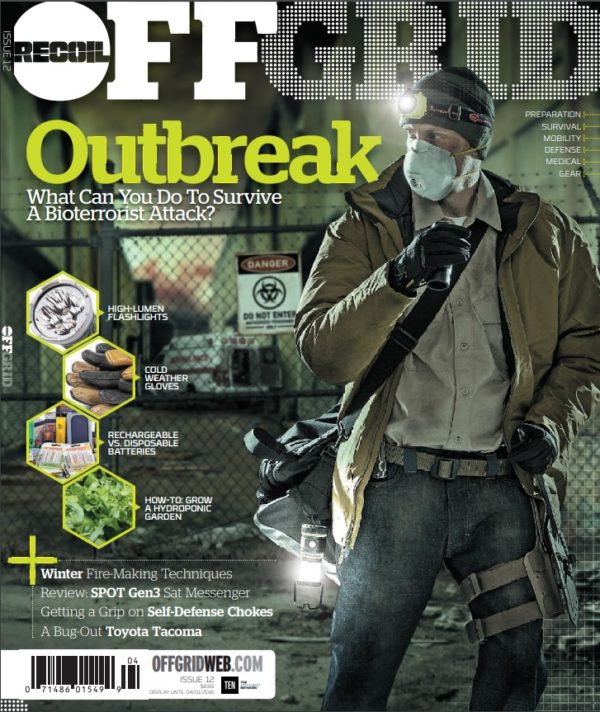
 STAY SAFE: Download a Free copy of the OFFGRID Outbreak Issue
STAY SAFE: Download a Free copy of the OFFGRID Outbreak Issue
No Comments