RECOIL OFFGRID Preparation Foot Care in Off-The-Grid Situations: When Your Dogs are Howling
In This Article
“A 1,000-mile journey begins with the first step.” It’s a sure bet that, off the grid, you won’t be spending a lot of time in your rocking chair. You’ll be up and about, sometimes traveling miles to perform the daily activities necessary to survive. You may need to carry heavy gear over rough terrain, scramble over obstacles, or sprint to escape danger. Foot care isn’t just a good idea — keeping your dogs from howling is absolutely necessary if you’re going to survive.
This is a general overview and not a comprehensive guide to treating foot injuries. Seek professional medical advice if you experience foot injuries that worsen over time.
The first lesson in Foot Care 101 is pretty much common sense: make sure your footwear fits. Many foot problems originate from poorly fitting shoes. There are lots of different brands of boots out there, and there’s no time limit for trying them on. Your shoes are arguably the most important article of clothing you’ll own in an off-grid scenario, so find the ones that fit best.
Heavier boots, like steel-toed, are great if you’re chopping wood (you get to keep all 10 of your toes) but are cumbersome for serious treks. Remember that an extra pound of weight in your boot is often compared to five extra pounds of weight on your back. Soft, flexible uppers will help.

Above: Boots must not only fit, but also be broken in. If you find a pair that works well for you, consider buying an identical backup set.
Hiking boots should be sturdy. Soles should be Vibram or other durable, high-traction material. In wet climates, waterproof layers like Gore-Tex are your friends. In warm climates, breathable boots can keep your feet cooler and drier. High-cut boots will help prevent ankle sprains by giving more support (and may even protect against the occasional snake bite).
Some people find the right boot but don’t “break it in.” Breaking in should be a slow, steady process, not a 15-mile hike the day after you bought them. Start by wearing them inside the house. Then, walk around the block a few times. Finally, put on a light pack and walk a short trail, slowly building up mileage and weight.
Another factor in keeping your feet healthy is your socks. Most people hike in the same pair of socks all day, even in the heat of summer. This can be extremely damaging to your feet. Sweaty feet are unhappy feet; wetness increases friction and gives you blisters. Change your socks often and have replacement pairs as a standard item in your backpack. Cotton socks retain moisture, but wool socks wick moisture away from the skin and even have antimicrobial properties to reduce odor. If you’re prone to blisters, consider the use of a lighter second pair of socks (sock liners) under the thicker hiking socks. Use foot powders, like Gold Bond, or even corn starch to keep your feet dry.
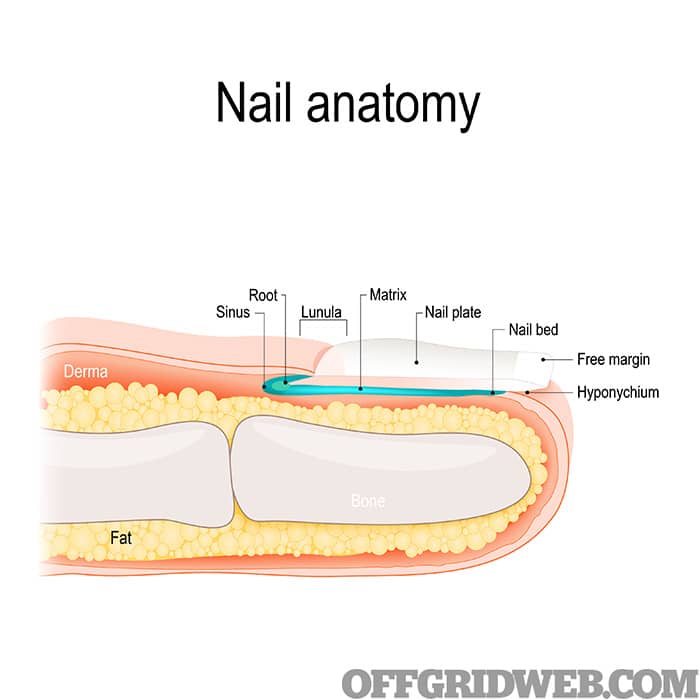
Above: A quick look at nail anatomy.
You’ve been a size 9.5 for as long as you can remember. Those 9.5s fit perfectly until one day … they don’t. What’s going on?
Believe it or not, it’s not abnormal for your foot size to change over time. As you walk, your body absorbs two to three times its weight due to gravity. The ligaments and tendons that support the arch in your foot become worn with use. As a result, the arch drops. The flattening that occurs causes your foot to become a little wider and longer. Extra weight as you get older has a similar effect.
Other age-related changes that affect foot care include the thinning of the fat pads that cushion the bottom of your feet. You might also develop bony changes like bunions, hammertoes, or other conditions that require more space.
Pregnancy also makes a difference. During pregnancy, there’s a big increase in a hormone called “relaxin.” This relaxes the pelvic bones and even makes it easier for the cervix to dilate during labor. It does the same to the ligaments in the foot, however, leading to changes in length and width that are often permanent.

Above: Failure to break in your boots may lead to big trouble. If you can’t walk, you won’t be able to do most other survival tasks.
Blisters: Blisters caused by excessive friction are, perhaps, the most common foot ailment off the grid. A foot blister is a small, often painful, fluid-filled pocket that forms on the uppermost layer of the skin. Blisters are filled with clear-to-yellowish liquid and can lead to infection.
Many rugged survivalists consider blisters to be no big deal, but they adversely affect work efficiency and need time to heal. An infected blister is a major issue and will become more swollen, painful, and red over the course of time. You might even develop a collection of pus called an “abscess.”
Usually, blisters occur as a result of choosing poorly fitting shoes, not having enough dry socks, or allowing your feet to become sweaty and wet.
Treating a blister first requires you to get off your feet. Wash your hands and clean the area thoroughly with an antiseptic like Betadine. The cleaner you start off, the less likelihood of infection.

Above: A large blister may require drainage.
Should you lance the blister? If it’s small, the answer is no, as an open blister is more likely to become infected. If the blister’s big, likely to break on its own, or very painful, however, some prefer to drain it. If so, follow these steps:
Athlete’s foot: Athlete’s foot (also known as “tinea pedis”) is an infection of the skin caused by a type of fungus known as Trychophyton. This condition may be a chronic issue, lasting for years if not treated. Although usually seen between the toes, you might see it also on other parts of the feet or even on the hands (often on the nails or between fingers). Athlete’s foot is contagious; it can be passed by sharing shoes or socks and even from wet surfaces such as shower floors. Those affected by athlete’s foot may also find themselves with other fungal problems, like “ringworm” or “jock itch” (Tinea cruris).
Any fungal infection is made worse by moist conditions. People who are prone to Athlete’s foot commonly have the same risk factors you might find in those who are thrown off the grid due to a disaster:
Athlete’s foot isn’t hard to diagnose. Look for flaky skin between the toes or fingers. The skin may appear red and the nails turn yellow. The patient will complain of itching and burning in the affected areas, sometimes severe. If the skin has been traumatized by scratching, you might see some fluid drainage. Often, the damage caused by the scratching is worse than the infection itself.

Above: Athlete’s foot (tinea pedis) is easy to diagnose but takes patience to treat.
If the condition is mild, keeping your feet clean and dry may be enough to allow slow improvement of the condition. Oftentimes, however, topical antifungal ointments or powders such as miconazole or clotrimazole are required for elimination of the condition. Don’t use anti-itching creams very often, however, as they keep the area moist and may delay healing. In the worst cases, oral prescription antifungals such as fluconazole (Diflucan) are needed.
Patience is a virtue when it comes to monitoring the healing process; it may take more than a month for a significant case of Athlete’s foot to resolve.
A favorite home remedy for Athlete’s foot involves putting tea tree oil liberally in a foot bath and soaking for 20 minutes or so. Dry the feet well and then apply a few drops onto the affected area. Repeat this process twice daily. Try to keep the area as dry as possible otherwise. For prevention of future outbreaks of athlete’s foot, apply tea tree oil once a week before putting on socks and shoes.
A quick mention of the old home remedy of urinating on your feet — if your urine has the usual concentration of a compound called “urea” in it, it probably won’t work. Dermatologists use stronger urea treatment with some success, however.
Corns: Corns are thick, hard patches of skin caused by friction that are found on the tops of toes. Some are barely noticeable but others may cause pain, especially when wearing ill-fitting shoes. Removing the source of friction may eliminate the problem. Other options include:
An ounce of prevention is worth a pound of cure. Corns may be prevented by wearing shoes that fit properly and using gel pad inserts to decrease pressure on vulnerable areas.

Above: Bunions and other conditions can cause a poor shoe fit (and pain).
Ingrown toenails: In the typical apocalypse movie, you’ll see gunshot wounds and broken bones, but in the real world, minor conditions can be a major problem. One of these is the ingrown toenail, also known as onychocryptosis.
While considered by some to be no worse than a blister or Athlete’s foot, ingrown nails can be severe enough to cause skin ulcers, blood infections (also called “septicemia”), or even total loss of circulation (“gangrene”).
Your fingernails and toenails are made up of a protein called keratin. It’s the substance that covers the claws, horns, and hooves of many animals. When we refer to issues involving nails, we refer to it as “ungual” from “unguis,” the Latin word for claw.
Nails consist of several parts. They include:
A toenail becomes ingrown when the edge of the nail grows into the skin of the toe. It can occur for a number of reasons, but poorly fitting shoes and poorly trimmed toenails are the most common causes. The big toe is usually affected, but any toenail can be affected.

Above: Ingrown toenails can become a serious problem due to how much pain they can cause.
The skin along the edge of a toenail that’s ingrown may appear red, swollen, painful, and even warm to the touch. These are signs not only of pressure on the skin, but also herald the beginning of an infection. If not treated, the condition worsens, possibly even leading to the drainage of pus.
Shoes that are either too tight or too loose can cause ingrown toenails. If too loose, it causes continual pounding of your big toe against the inside due to movement within the shoe as you walk. With shoes that are too small for your foot (or even high heels), extra pressure is placed on your toes that prevents normal nail growth.
Nails that aren’t trimmed properly can also cause ingrown toenails. This happens when your toenails are trimmed too short, or you cut your toenails in a rounded fashion instead of straight across. Rounded cuts are appropriate for fingernails, but not toenails. The edges of the nails will tend to curl downward and grow into the skin.

Above: Corns are caused by repeated friction or pressure.
Some people are born with nails that are curved and naturally tend to curve inward. Injuries to the nail bed can also cause ingrown toenails, especially if it affects the germinal matrix, the living part of the nail that produces new cells. People with diabetes or other illnesses that cause poor circulation are also at higher risk for these problems. A diabetic, for example, may experience nerve damage and not realize that excessive pressure is being applied to the toes by ill-fitting shoes. They may not even notice that the nail is growing into the skin.
In some cases, an ingrown toenail can be treated by:
At some point, however, you may have no choice but to intervene more aggressively. In these circumstances, remove the offending segment of nail. Remove the side trapped under the skin by using a scalpel or clippers, about 1/5 of the nail width or less. You may have to cut all the way down to the base and use a clamp for removal. Expect some bleeding.

Above: Blisters are a common result of ill-fitting shoes.
As you might expect, this procedure is more easily done after injecting local anesthetic (plain lidocaine) into the area. Be aware that if a portion of the nail is removed, it may take months for it to regrow.
If the toe is infected, antibiotics might be appropriate. Triple antibiotic ointment may be helpful here, but oral antibiotics, such as cephalexin, clindamycin, or amoxicillin may be necessary.
If a portion of the nail is cut off, patience is required as it’ll take months for the nail to regrow. If you have a genetic tendency toward ingrown toenails, be prepared to deal with recurrences.

Above: Hammertoes are age-related changes that require more space in shoes and boots.
There are various types of toenail injuries. Amputations and fractures may occur due to trauma, but more commonly you’ll see:
Nail bed lacerations: In a nail bed laceration, the nail and underlying tissue is cut. This may occur as a result of a knife or a crush injury. These wounds will bleed and leave bruising that may take a long time to heal.
Nail bed avulsions: An avulsion occurs when your nail and nail bed is pulled off the toe. This can occur when a toe is jammed into a tight space but may be caused by various other traumatic events. This injury is very painful; it has even been used as a form of torture.
Subungual Hematomas: When bleeding occurs under the nail plate, it’s often trapped and accumulates, forming what is called a “hematoma.” It’s the classic result of hitting your finger with a hammer. You can expect throbbing pain and some bruising. When a significant amount of blood accumulates, it may lift the nail plate.

Above: Some nail lacerations may require closure with stitches.
In normal settings, an X-ray is often performed to rule out a fracture of the digit. You won’t have such modern medical technology available off the grid. Some procedures may be performed with a good medical kit and supplies. In the case of an avulsion or laceration:

If a crush injury causes a bruise (also called an “ecchymosis”), it’ll be painful but usually just for a short time. In this case, some ibuprofen or other pain med should help. A hematoma will continue to be painful, however, even several hours after the event. A bruise is likely to appear brownish or blue, but a hematoma may appear a deep blue-black.
If very painful or significant blood has accumulated under the toenail, a further procedure called “trephination” may be performed. In this instance, a very fine drill (or a red-hot 18-gauge IV needle or paper clip) is used to make a hole in the nail plate large enough to drain the blood and relieve the pressure under the nail. This is an important consideration to avoid damage to the nail bed. In the worst cases, the nail plate is removed instead.

Above: A subungual hematoma appears bluish-black and painful.
The toe must be kept clean, dry, splinted, and bandaged for a minimum of 48 hours afterward. Most inexperienced medics should avoid this procedure except in the most severe cases, as the pain will usually decrease over time even if you do nothing.
It’s important to know that damage to the base of the nail (the “germinal matrix”) may be difficult to completely repair, and that the fully healed nail may look irregular in some way. A completely torn-off nail will take four to six months to grow back.
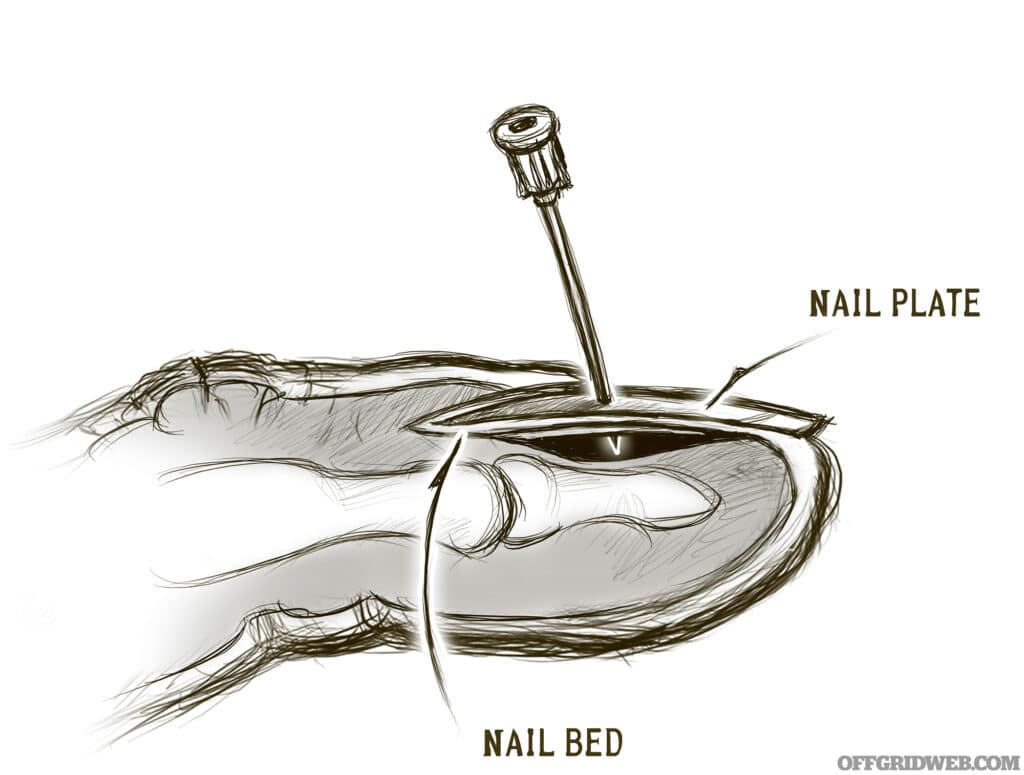
Above: Trephination can eliminate painful hematomas under the nail.
Online shopping is the norm for many these days, but not the best strategy when it comes to purchasing shoes. There are some simple ways to make sure you’re buying shoes that will fit and serve you well for years:

Above: Removing the roof of a drained blister exposes the sensitive flesh beneath. For added protection, it might be best to leave the outer layer of skin in place.
If you’ve found the right boot, consider getting a second pair (and breaking them in also).
Each part of your foot should be happy in your new boots:

Above: When trying on boots, use the socks you’d wear with them.
Joe Alton, MD, is a physician, medical preparedness advocate, and New York Times/Amazon-bestselling author of The Survival Medicine Handbook: The Essential Guide For When Help Is NOT On The Way, Alton’s Antibiotics and Infectious Disease, Alton’s Pandemic Preparedness Guide, and other books. He designs survival medical kits at store.doomandbloom.net.
Don't forget to subscribe to Recoil Offgrid's free newsletter for more content like this.
 STAY SAFE: Download a Free copy of the OFFGRID Outbreak Issue
STAY SAFE: Download a Free copy of the OFFGRID Outbreak Issue
No Comments