RECOIL OFFGRID Survival DIY Disinfectants: How to Fight Diseases with Limited Resources
In This Article
Maintaining the health of an off-grid community involves suppressing infections and keeping wounds clean. For these, you’ll need antibiotics to destroy bacteria within the body and antiseptics for use on the skin. More, however, is needed to assure you’ll avoid contamination that could lead to epidemic disease among your people: you’ll need disinfectants. A disinfectant is a substance used to eliminate disease-causing organisms (called “pathogens”) on inert surfaces such as countertops and medical instruments. If these surfaces aren’t disinfected, they can be teeming with germs. Contaminated instruments and sick room surfaces can get the entire group infected. The off-grid medic needs to have disinfectants on hand that can assure the health and safety of the people in their group.
Some disinfectants do double duty as antiseptics, but many are too harsh to apply to living skin, and, certainly, too strong for internal use. They work just fine, however, on work surfaces and other inanimate objects.
Disclaimer: This article is meant to be a brief overview and not a detailed guide on creating disinfectants. Seek professional medical help before attempting any of the steps outlined in this article.
Above: Boiling water eliminates enough microbes to allow it to be used in wound care.
A significant factor in the quality of medical care given off the grid is the level of cleanliness of the equipment used. You may have heard the terms “sterile” and “clean.” What’s the difference?
When it comes to medical protection, “sterility” means the complete absence of microbes. Sterile technique involves hand washing with special solutions and the use of sterile instruments, gloves, towels, and dressings. The “sterile field” is isolated to limit contact with anything that could allow micro-organisms to invade it.
Above: Work surfaces must be regularly disinfected.
It’s very difficult to achieve a “sterile field” if you’re in a remote environment. In this case, we may only be able to keep things “clean.” Clean techniques concentrate on reducing, as much as possible, the number of microorganisms that could be transferred from one person or object to another. Work surfaces must, at least, be clean or they will increase the risk of infection. Organism-containing dirt or droplets from coughing or sneezing regularly contaminate these areas.
Once visible dirt is cleaned off a surface, disinfectant solutions may be applied for what is called the “contact time.” The contact time is the time that the disinfectant must remain visibly wet on a surface to ensure full effectiveness. This time period is based on the results of Environmental Protection Agency (EPA) testing. Instructions regarding contact times are usually printed on the product label. The maximum contact time for a Food and Drug Administration (FDA)-approved disinfectant cannot be more than 10 minutes.
Many commercial disinfectants will be scarce in a long-term disaster. There are some widely available options, however, that can be stockpiled or improvised. Be aware that each type may vary in its effectiveness against specific organisms.
ALCOHOL
From the medic’s standpoint, the two alcohol compounds useful for disinfection are ethyl alcohol and isopropyl alcohol. These alcohols kill bacteria rapidly, although they may not be enough to destroy “spores.” A spore is a resistant form adopted by some bacteria in adverse conditions.
Above: 80-proof liquor is only 40-percent alcohol, not enough for disinfectant purposes.
Alcohol has the benefit of also being effective against viruses, fungi, and variant types of bacteria such as tuberculosis. As a disinfectant, however, alcohol’s action drops sharply when diluted under 50 percent. The optimum bactericidal concentration is 60 to 90 percent in water. The amount found in liquid hand sanitizers is usually 60 to 70 percent. A bottle of rubbing alcohol usually contains 70 percent. The amount found in 80-proof whiskey is only 40 percent, thus failing the criteria for a potent disinfectant. When spirits must be used as disinfectants, most choose 100 proof (50 percent) vodka kept wet on a surface for at least 30 minutes.
Above: Hand sanitizers should contain at least 60- to 70-percent alcohol.
The risks of using alcohol compounds to sterilize instruments include eventual damage to rubber, plastic, and other parts. Another issue is the flammability: They must be stored in a cool, well-ventilated area. Alcohols also evaporate rapidly, so you must have enough to fully immerse an instrument you want to disinfect.
CHLORINE SOLUTIONS
Chlorine solutions made from sodium and calcium hypochlorites can be powerful disinfectants. Sodium hypochlorite is available in liquid form as household bleach; calcium hypochlorite is available in various solid pool-cleaning products. Both quickly eliminate a broad array of microbes, don’t leave toxic residues, and are relatively inexpensive. Extended-release chlorine dioxide is another option which has a more prolonged effect.
Above: One part household bleach in nine parts water yields a strong disinfectant solution.
Hypochlorites are widely used for disinfecting. A 1:10 dilution of standard household bleach has been recommended for decontaminating blood spills. Full-strength bleach has been recommended for self-disinfection of needles and syringes used in needle-exchange drug programs.
In addition to skin and eye irritation, chlorine solutions can produce corrosion in plastic and metal instruments over time. When mixed with ammonia, it can produce a toxic gas.
Another issue with chlorine solutions is their longevity. If stored in an opaque container, they can last several months to a year. Left out in the open, however, they lose potency very quickly.
To make a chlorine solution with the pool cleaning agent calcium hypochlorite:
FORMALDEHYDE
Formaldehyde is sold as a water-based solution called formalin, which is 37-percent formaldehyde by weight. The solution kills bacteria, fungi, viruses, and spores.
Varying concentrations of aqueous formaldehyde solutions are needed to destroy different microorganisms. For example, almost all viruses are inactivated rapidly with a 2-percent formalin solution. Higher concentrations and longer exposures are needed for certain bacterial spores, like anthrax.
Formaldehyde is highly toxic to living tissues. Ingestion can be fatal. Long-term exposure to low levels in the air or on the skin can cause asthma-like symptoms and skin irritation. One advantage of formalin is a relatively long shelf life of at least two years.
HYDROGEN PEROXIDE
Hydrogen peroxide has good germicidal activity against bacteria, viruses, spores, and fungi. The drug store version is 3-percent concentration, but stronger versions of food-grade hydrogen peroxide are available.
Above: Hydrogen peroxide mixed 1:1 with water can be effective.
The time required for inactivating common-cold viruses using a 3-percent hydrogen peroxide solution is about six to eight minutes. For disinfectant purposes, a 7-percent concentration works more rapidly. Toxicity is not usually an issue unless ingested. In fact, a 1:1 dilution of household hydrogen peroxide and water has been used as a mouth rinse.
Under normal conditions, hydrogen peroxide is extremely stable when stored in dark or opaque containers, lasting three years or more if unopened (six months if opened).
IODINE SOLUTIONS
Iodine solutions have been used by health professionals primarily as antiseptics on skin or tissue. Iodophors, on the other hand, have been used both as antiseptics and disinfectants. An iodophor is a combination of iodine and a “carrier”; the resulting complex provides a sustained-release reservoir of iodine and releases small amounts of free iodine in water. The best-known and most widely used iodophor is povidone-iodine, a compound of polyvinylpyrrolidone with iodine.
Above: Betadine, a combination of iodine and povidone, has been used as a disinfectant and antiseptic.
Betadine is the most well-known iodophor brand. It’s used most commonly as a 10-percent solution which contains only 0.001-percent free iodine. This product retains the germicidal activity of iodine, but is relatively free of toxicity if not ingested.
“Free” iodine is the main contributor to the bactericidal activity of iodophors. Surprisingly, a dilute iodophor demonstrates more rapid bactericidal action than does a full-strength one! The reason is not entirely clear, but dilute solutions seem to cause more free iodine to emerge.
Povidone-iodine solution has a published shelf life of two to three years. Unopened bottles may last longer.
Above: Various common household products can serve as disinfectants.
While not as powerful in antimicrobial action as commercial disinfectants, certain natural products have beneficial action against germs:
Above: Vinegar has been used as a disinfectant, but isn’t as strong as some others.
Pressure Cookers – An Autoclave Alternative
Above: Instruments can be disinfected using a pressure canner.
You won’t have an autoclave, but having a pressure cooker/canner as part of your supplies will allow instruments to achieve the level of sterility required for minor surgical procedures. You’ll need to achieve 15-20 psi (250 degrees Fahrenheit) for at least 20 minutes. Here's a step-by-step guide to using a pressure cooker to sterilize instruments:
Pressure cookers, if used incorrectly, can cause severe burn and scalding injuries. Be sure to have a working knowledge and experience using them (read your manual).
Ultraviolet Radiation
A significant development in the quest to sterilize medical instruments off the grid comes from a recent study commissioned by the military. The study, published in the journal “Wilderness and Environmental Medicine,” explored the use of UVC light as a survival medical tool.
Above: Using UVC light as a disinfectant starts with scrubbing an instrument with chlorhexidine (Hibiclens).
In this study, instruments laden with MRSA and other bacteria were first scrubbed with Chlorhexidine (Hibiclens) antiseptic for 30 seconds and dried with a sterile gauze 4×4-inch pad. Then, a battery-powered ultraviolet C (UVC) wand was passed within 4 inches all over the instruments for 45 seconds.
Evaluation afterwards revealed a 100-percent reduction of bacteria and achieved levels of sterilization acceptable for use in the field. If the instruments were not used right away, rapid vacuum sealing extended the life of sterility.
Above: After cleaning with chlorhexidine, pass a UVC wand completely around the instrument for 45 seconds.
Strict attention to hygiene and disinfection will save many lives in the aftermath of a disaster. It takes someone willing to stockpile and improvise ways to keep their people healthy in such a scenario. If that person succeeds, a major catastrophe can be just a bump on the road, not the end of the road, for their family or group.
Joe Alton, MD is a physician, medical preparedness advocate, and Fellow of both the American Colleges of Surgeons and OB/GYN. He is the author of the Book Excellence Award winner in medicine, The Survival Medicine Handbook: The Essential Guide For When Help Is NOT On The Way and other books. He is also the designer of an entire line of quality medical kits at store.doomandbloom.net and altonfirstaid.com.
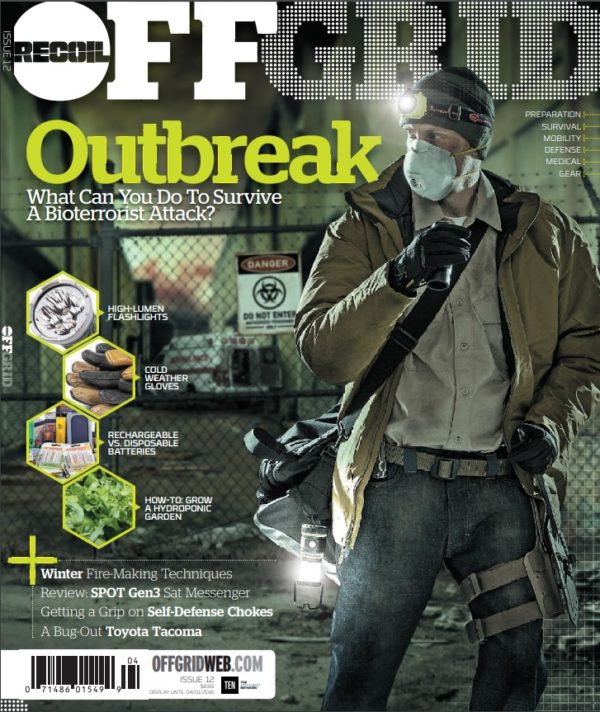
 STAY SAFE: Download a Free copy of the OFFGRID Outbreak Issue
STAY SAFE: Download a Free copy of the OFFGRID Outbreak Issue
No Comments