RECOIL OFFGRID Survival PTSD
In This Article
Somewhere between 3 to 8 percent of the population will deal with Post Traumatic Stress Disorder, or PTSD, in their lifetime. In the past 30 years, progress has been made in identifying therapies to aid in the recovery of individuals afflicted by PTSD. Several treatment modalities have shown benefit. The purpose of this article is to review some of those treatment modalities. We hear more about PTSD today due in part to its fairly recent recognition by several organizations as a “real” psychiatric disorder as well as increased public service announcements.
A lengthy and specific definition of PTSD can be found in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). To summarize, people who have PTSD are often those who have undergone a traumatic experience related to near death or perhaps a trauma related to sexual abuse. They often have flashbacks, distressing dreams, or memories of the traumatic event. Because of these symptoms, patients may avoid anything that reminds them of the event.
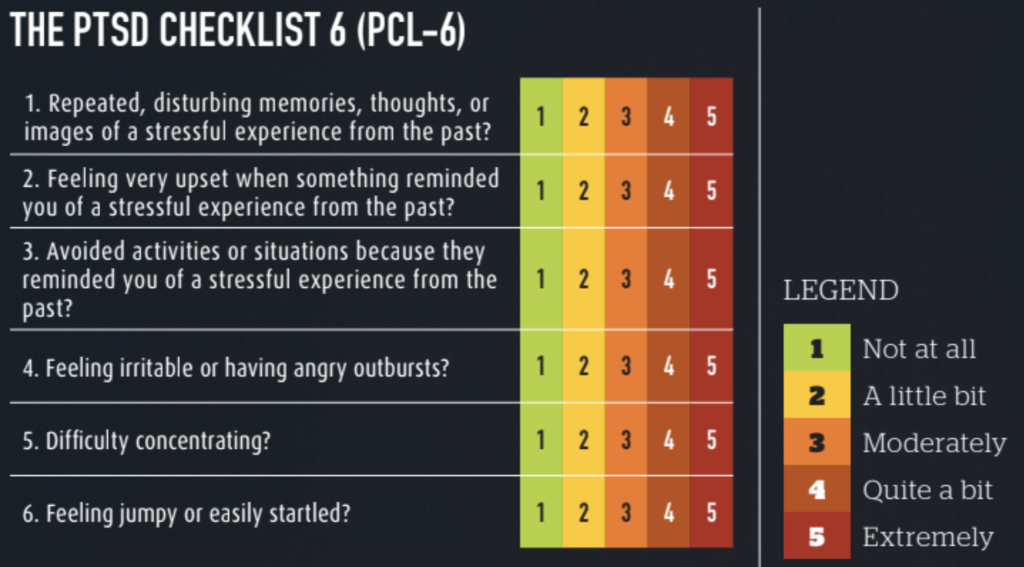
These experiences cause a variety of symptoms, including anxiety, irritability, disruptive behavior, depression, isolation, and even suicidal thoughts. We now have a common screening assessment for PTSD, called the PTSD Checklist (PCL). There’s a version for civilians (PCL-C) and one for military (PCL-M). If you score above 44 on the PCL-C, or 50 on the PCL-M, you may have PTSD, and need to see a doctor for further recommendations. A shorter version is the PCL-6, where a score of 14 or greater suggests that PTSD is likely.
A physician may prescribe medication, psychotherapy, or both to assist in treatment. Studies have shown that these are about 50-percent effective in helping those with symptoms of PTSD — not perfect, but every bit helps. Medication stabilizes the mood and lessens some of the symptoms that are disrupting the individual’s life. Therapy is an essential adjunct to help the person overcome the negative associations and psychological pain attributed to the event.
Drugs like Selective Seratonin Reuptake Inhibitors (SSRIs) and Seratonin-Norepinephrine Reuptake Inhibitors (SNRIs) are the standard of care for PTSD. SSRIs include drugs like Sertraline (Zoloft), Fluoxetine (Prozac), and Paroxitine (Paxil); Venlefaxine (Effexor) is a recommended SNRI. These drugs work on chemical components of the brain that help the patient deal with anxiety and depression that’s often experienced with PTSD.
Another drug that has been helpful in some patients with PTSD is Prazosin. This drug is commonly used to treat enlarged prostate in men; however, it has been shown in some people to reduce the number of nightmares and improve quality of sleep. Study conclusions have been mixed as to Prazosin’s general effectiveness; however, it’s typically recommended to see if there’s a benefit in each individual patient.
Lastly, medical marijuana has gained a lot of popularity for treating just about everything under the sun; however, it hasn’t been shown to provide a benefit in PTSD patients.
Jon Kabat-Zinn wrote his treatise on mindfulness back in 1990, detailing what mindfulness is and how to go about being mindful. In short, he proposed that we become mindful of the moment. Savor the food we chew. Feel the sun on our face and the grass beneath our feet. In doing so, we can gain an appreciation of our current moment and live a better, more in touch, life.
Often with PTSD, the trauma keeps rearing its ugly head, and we forget about the moment we are living, and step back into a horrible time in our lives. Mindfulness offers an escape from the past as we focus on the now. There’s an excellent app called Mindfulness Coach that I recommend. Also check out www.mindful.org to learn more about mindfulness.

Above: Mindfulness and meditation are essential components of PTSD treatment.
Eye Movement Desensitization and Reprocessing (EMDR) was developed by Dr. Francine Shapiro in 1990. It’s a complex form of therapy that combines modalities from other therapies to have its beneficial effects. Basically, in EMDR, the traumatic event is recalled while a repetitive act is performed (tapping fingers, roving eyes). This interrupts the old thoughts associated with the memory and creates a new pathway for the brain to associate with the event. The process can take a while to prime the patient for successful treatment. It has a lot of research showing its benefit, as supported by the World Health Organization, the American Psychiatric Association, and the Veterans Administration. I have seen this work in several patients with amazing success. See www.emdr.com for more information.

Above: Physicians should take a multi-disciplinary approach to treat PTSD.
The idea of using medication injected into the stellate ganglion on the right side of the neck was first proposed in the 1940s. It wasn’t until 2010 that the first study was done to see if stellate ganglion block could help with PTSD. Although the exact mechanism of how it works is unknown, the idea is that it “calms down” sympathetic stimulation of the nerves during anxious times. It’s still being used, but there’s mixed evidence that it’s helpful. The Veterans Administration suggests that more study needs to be done on this modality.
This popular and effective therapy focuses on the symptoms of trauma and its effects on thoughts, feelings, and behaviors. There are two modalities commonly used in CBT: exposure therapy and cognitive restructuring. In exposure therapy, the person might be asked to relive the trauma in a safe environment. The exposure can be written, verbal, or even virtual reality-based. In cognitive restructuring, the person is asked to recall the trauma in a more logical way, as they often only remember pieces of the trauma and sew together what they may have missed. The goal is to have the patient re-evaluate their negative associations with the trauma and to develop more effective patterns of thought. There are typically 12 to 16 sessions involved.

Above: Cognitive Behavioral Therapy has been proven to be effective in treating PTSD.
This was developed in the 1980s and is a specific subset of Cognitive Behavioral Therapy aimed at treating those who have succumbed to a sexually traumatic experience. Often, patients blame themselves after such an incident. Patients are asked to think about their trauma and how it has affected them. In order to overcome their trauma, they must develop an understanding of how they feel in relation to the trauma. They must develop new patterns of behavior associated with the event (e.g. “I survived the trauma because I fought the SOB,” rather than “How did I let this happen?”). CPT is typically 12 sessions long.
Post-Traumatic Stress Disorder affects millions of people in the U.S. Our understanding of screening, diagnosis, and treatment has improved over the past 30 years. PTSD is now recognized by the American Psychiatric Association and the World Health Organization as a disease. Medications and relatively newer therapies, such as Eye Movement Desensitization and Reprocessing, as well as older therapies, such as Cognitive Behavioral Therapies, can provide benefits to people afflicted with PTSD. Treatment is lifelong, and there are no shortcuts. There is help, and there is hope, for those suffering with PTSD.
David L. Miller, DO, FACOI, is an internist in private practice for 20 years. His experiences away from the office have included time as a fight doctor in regional MMA events and as a team physician for 10 years at a mid-major university in the Midwest. Currently, he serves as the lead medical instructor for the Civilian Crisis Response team based out of Indianapolis.
 STAY SAFE: Download a Free copy of the OFFGRID Outbreak Issue
STAY SAFE: Download a Free copy of the OFFGRID Outbreak Issue
No Comments