RECOIL OFFGRID Survival The Myths of Dealing With Frostbite
In This Article
Disclaimer
This article is meant to be a quick overview and not a detailed guide on how to deal with frostbite in an emergency situation. Professional medical treatment should always be sought first before attempting any of these methods.
Subfreezing temperatures and biting winds are a recipe for disaster, particularly when you find yourself ill-prepared and suffering from the onset of frostbite. When you're stuck outdoors, there's a lot riding on your choice of emergency treatments. But will you make the right choice?
The Myth: Since friction generates heat, and it's instinctive to rub an injury, it only seems logical that we should rub frostbitten skin to thaw it out. People also have a habit of using hot or scalding water to defrost frostbitten/frozen tissue and thawing tissues, which are still under the threat of refreezing. Unfortunately, each of these ideas can lead to painful and permanent consequences.
The Reality: When the mercury drops below 32 degrees F and exposed skin starts to freeze, there are a number of mistreatments that'll exacerbate winter injury. Here we'll dispel some of the myths associated with proper frostbite treatment.
Frostbite occurs when ice forms in your skin and the underlying tissues. Superficial frostbite frequently happens to exposed skin (typically the face), but it can also affect the ears, hands, and feet (particularly fingers and toes). This lightly frozen tissue may appear waxy and pale, feeling stiff on the surface, but the underlying tissue still feels soft. Pain or numbness will likely accompany the aforementioned symptoms.
If the frostbite is severe, freezing can strike deeper tissue across a wider area. This extreme form will cause skin to appear pale and firm, and underlying tissue to feel solid. Tissues with deep frostbite will generally feel numb and joint movement will be restricted. Severe frostbite could result the loss of appendages due to infection and necrosis (tissue death).
The proper treatment of frostbite is gentle, gradual rewarming of the skin and tissues. This can be done both in the field and in the hospital, but should only be attempted if there's no danger of refreezing.
For any frostbite treatment, first seek shelter from the cold. Then prepare for the intense pain by taking Ibuprofen, unless you're allergic to this medication. For superficial frostbite, place a warm body part against the frostbitten tissue. This could mean placing your frosty foot against your friend's warm belly or tucking your own fingers under your bare armpit. Rewarm the tissue until it is soft and the color has returned.
Deep frostbite requires gradual rewarming of the tissue using warm water at stable temperatures. Use a thermometer to make sure the water isn't over 105 degrees F. And if a thermometer isn't available, use an uninjured body part to gauge the temp. Using a suitable container, slowly immerse the frosty extremity. Add more warm water as needed to maintain the water temperature in the container. If possible, pre-treat with pain meds before you begin rewarming (consult your doctor before taking higher-than-normal doses of any meds). Advil and Motrin are other alternatives that can be used to reduce pain. And resist your temptation to rub or massage frostbitten areas — this will only result in more tissue damage.
Once thawed, do your best to protect yourself or your frostbitten patient from refreezing, and monitor for hypothermia and shock. Continue your care with Ibuprofen every eight hours until you or the person suffering frostbite can receive proper medical care. Eat foods high in calories and protein to fuel the body and restore your overall temperature. Finally, avoid smoking and alcohol after this kind of injury.
Avoidance: Prevention is the best strategy. Cover your exposed skin with garments capable of blocking wind. Temperatures that are barely below freezing can still lead to frostbite when strong winds are involved (or if you have been exposed to the cold for a long period). The threat grows as temperatures drop near 0 degrees F with any wind. Frostbite can occur on exposed skin in mere minutes when the temperature is below 0 degrees F and the winds are over 20 mph.
Know the Location: Frostbite typically first affects the extremities that have minimal blood flow. Just remember this rhyme, “fingers, toes, ears, and nose.” This can help you remember to check these areas frequently for blood flow and warmth during your outdoor travels. Check capillary refill by squeezing fingers and toes, then watching how quickly the blood returns after letting go.
Time Will Tell: If you were stranded in a remote area and experienced severe frostbite, it only takes a few days for skin to blister and begin turning black. A week or two after the injury, frostbite shifts to necrosis, which will likely lead to massive infection. Deep frostbite is an unbelievably painful condition with a high rate of infection. Even after weeks or months of medical care, the frostbitten tissue can still be at risk. As the ice crystals form in healthy cells, the jagged points pierce and stab the cell — killing it and even neighboring cells. These areas are laden with dead tissue that often turns black and requires surgical removal. Daily care is necessary for weeks after a moderate to severe frostbite occurrence. Skin grafts and amputations can still occur even a month after the initial injury. Always seek professional medical care as soon as possible if you've experienced frostbite.
Don’t miss essential survival insights—sign up for Recoil Offgrid's free newsletter today!
Read articles from the next issue of Recoil Offgrid: Issue 25
Read articles from the previous issue of Recoil Offgrid: Issue 23
Check out our other publications on the web: Recoil | Gun Digest | Blade | RecoilTV | RECOILtv (YouTube)
Editor's Note: This article has been modified from its original version for the web.
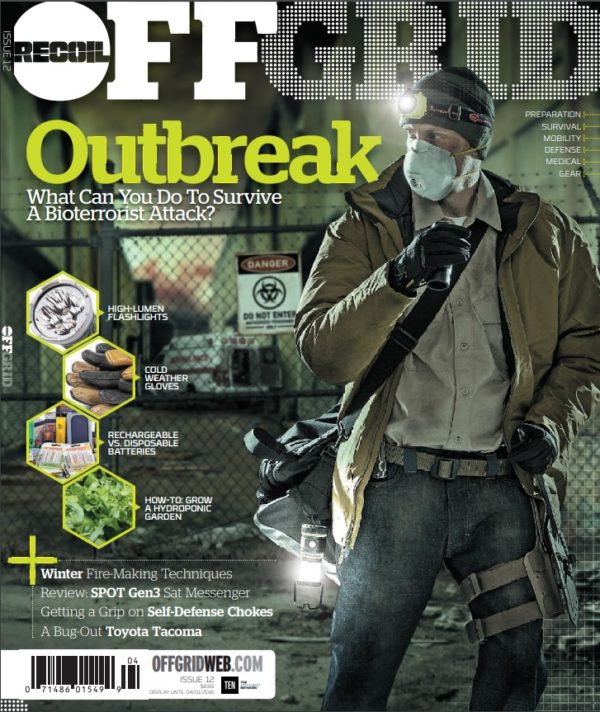
 STAY SAFE: Download a Free copy of the OFFGRID Outbreak Issue
STAY SAFE: Download a Free copy of the OFFGRID Outbreak Issue
No Comments