RECOIL OFFGRID Survival Traumatic Shock Treatment & Survival
In This Article
WARNING: This article is meant to be a quick overview and not a detailed guide on how to deal with shock in an emergency situation. Professional medical treatment should always be sought first before attempting any of these methods.
Shock has many different possible meanings. You could be shocked at the turn of events in a movie. You could be shocked by touching a live wire. You could be in shock after receiving news of the death of a loved one or due to trauma. For me, shock is a chilling term that portends poor outcomes despite our best medical efforts. Mortality can be 40 to 50 percent, despite the best medical care in the best hospitals. What will you do if your partner or family member has an accident or heart attack and goes into shock? Perhaps the most important part of treating shock is learning to identify it as soon as possible. The earlier the identification, the earlier the treatment can begin.
First off, shock is essentially a lack of blood and oxygen supply to the tissues. The lack of these nutrients causes tissues and cells to starve. When this occurs, the tissues and organs lose function. The more organs that fail, the higher the mortality rate. The sooner the cells can restore their nutrients and function, the better the chance of survival.
The body has several mechanisms to attempt to compensate for the lack of tissue perfusion in order to minimize the damage to the cells. Although many organ systems are involved in the compensatory mechanisms, it’s the cardiovascular system that’s the foundation of the process. In order for the cardiovascular system to maintain its pressure in a closed loop, there has to be a pump (the heart), pipes (the blood vessels), and fluid (the blood). If there’s something wrong with any one of these components, then there’s a loss of pressure in the system. If that loss of pressure is severe, the tissues and organs won’t be nourished with the essential components that allow for proper function of the organs and our body.
Let’s look at this in a little more detail. The pressure in the system is controlled by the output of the pump (cardiac output) and the systemic vascular resistance (changes in vessel diameter or changes in blood viscosity). The cardiac output is determined by the heart rate and the stroke volume (how much blood is pumped out with each contraction of the heart). The equation is as follows:
In order to raise the pressure in the system, we need to increase heart rate, increase stroke volume, or increase systemic vascular resistance (or some combination of the three). What often happens in an injury or disease is that one of these components falters and the other two attempt to compensate. This equation is paramount to understand what’s happening physiologically to someone in shock.
With that in mind, the symptoms of shock should make sense. Hypotension (low blood pressure) is prevalent. The person may experience extreme fatigue, dizziness when standing, or faintness. Low blood pressure causes the body to shunt blood away from less essential organs like the skin. The skin becomes pale and cold. In order to attempt to compensate for the low blood pressure, the heart rate increases. This pushes the blood faster around the system to utilize the remaining oxygen within the system. The respiratory rate increases to bring more oxygen into the system and to lessen the effects of increased acid buildup from lack of tissue perfusion. A person may become disoriented or confused due to lack of blood or oxygen to the brain.
The whole process can develop rapidly and has three stages to focus on. The first stage is the initial, or pre-shock, stage. This is the moment an injury occurs to the person. In an example of trauma, blood is being lost through a wound. This is essentially a decrease in the stroke volume from the equation above. This in turn decreases the cardiac output. The body will attempt to compensate by increasing the heart rate and increasing the systemic vascular resistance (via vasoconstriction). The latter mechanism attempts to control the bleeding and shunt blood away from less essential tissues.
In the second stage (compensatory stage), the body continues to minimize the damage being done. This stage is reversible (by acting quickly, there’s a good chance tissue and organs can be saved). The body activates the sympathetic nervous system due to the decreased cardiac output, and hormones such as epinephrine are released to increase the contractility of the heart. When the body fails to compensate, the progressive stage ensues. This is where the tissues suffer increased ischemic damage, and lactic acid builds up in the bloodstream. The further along this stage goes, the more likely it becomes irreversible and organs start to fail. Urine output drops initially as the body tries to retain all the volume it can. Later, urine production stops due to the death of cells in the kidney. The liver fails, which causes a disturbance in the coagulation cascade, and it’s easier to bleed. Death is imminent.
So, with the physiology of shock outlined above, let’s look at how that physiology is affected by various causes of shock. There are two different classifications of shock: differentiated and undifferentiated. Many times when someone is in shock, we say it’s undifferentiated because the patient exhibits signs of shock, but we may not know the exact cause. We start treatment protocols immediately because time is off the essence. When we do know what is causing the shock (differentiated shock), we break it into four general categories: distributive, cardiogenic, hypovolemic, and obstructive.
Referencing the aforementioned equation, distributive shock is where the systemic vascular resistance decreases, and blood vessels generally dilate. The body tries to compensate by increasing the heart rate. We further break distributive shock down into septic and non-septic causes. Sepsis is the effect of the body’s response to infection. Common sources of infection are urinary tract infections, pneumonia, and even skin infections. With treatment in the hospital setting, the mortality is roughly 40 percent. For non-septic causes of distributive shock, mortality depends on the initial insult.
There are four categories of non-septic distributive shock: inflammatory, neurogenic, anaphylactic, and “other.” The inflammatory portion could also be a component of sepsis, or could be associated with a severe burn, trauma, or heart attack. Neurogenic shock is usually due to a spinal cord injury or traumatic brain injury. The autonomic nervous system is altered, leading to decreased systemic vascular resistance and unopposed vagal tone.
Because of these changes, the distinguishing feature of neurogenic shock is usually a slow heart rate, which makes it difficult for the body to compensate. Anaphylactic shock can be caused by food allergies, environmental allergies, medication allergies, or idiopathic reasons.
Injectable epinephrine at the onset of anaphylaxis is critical to survival. Venomous stings (e.g. bees, scorpions, and snakes) are often considered in the “other” category. Interestingly, carbon monoxide, myxedema (due to extreme hypothyroidism), and narcotics are also included in this category due to their effect on systemic vascular resistance.
In a survival setting, many of the causes of distributive shock could be prevented or prepared for prior to the irreversible portion of shock. Carrying antibiotics and keeping wounds clean can minimize risk of infection. You could also try eating garlic or onion at the first sign of infection. This won’t do anything once you’re very far into the pre-shock stage, though. You could also try apple cider vinegar, Echinacea, hydrogen peroxide, or turmeric to help keep a wound clean. Keep in mind that these are very early interventions. Readily available epinephrine for anaphylaxis is a no-brainer, especially if you know you have such reactions. If you have a thyroid condition, ensure that you have enough medication. People who are on chronic steroids must also ensure they don’t run out of these, or they risk adrenal insufficiency, shock, and death.
This occurs when there’s a loss of fluid and, in essence, a decrease in stroke volume due to the loss. In order to maintain blood pressure, the heart rate increases to maintain cardiac output, and the arteries constrict to maintain systemic vascular resistance. There are two classifications in hypovolemic shock: hemorrhagic and non-hemorrhagic. In hemorrhagic shock, there’s a disruption of the vascular system, causing a leak. While this can be easily identified by severe external bleeding, don’t forget that internal hemorrhage may not be as apparent.
This could be due to blunt force trauma that causes a rupture in an organ such as the spleen, or a tear in a major vessel from a motor vehicle crash. Pelvic fractures are also known for internal bleeding. Look for bruising on the abdomen or flank, as well as for abdominal distention, as potential indicators of hemorrhage. Stabilizing a pelvic fracture at the scene when there’s evidence of internal bleeding or shock can help slow the hemorrhage. You could consider using a sheet, blanket, or the SAM Pelvic Sling.
Remember that people on any type of blood thinner, including aspirin, are at increased risk of more significant bleeding. Other treatments involve stopping the bleeding by holding pressure to obvious sources of bleeding. If a tourniquet is needed for injuries to the extremity, apply it if you have the proper training on their use. Coagulant powder is also an option. If you don’t have any, remember that cayenne pepper, turmeric, juniper sap, and other natural remedies could also help. Because you might be miles from help, the key is to stop the bleeding rather than replace the fluids.
In non-hemorrhagic shock, the loss of total body water is profound. Because of the water loss (as opposed to blood loss), the viscosity of the blood increases, and thus systemic vascular resistance increases. Fluid loss can be severe due to vomiting and/or diarrhea due to enteritis from bad food or water. Heat stroke can also cause profound dehydration, leading to shock. Mortality for heat stroke can be as high as 80 percent if it’s not treated promptly.
In cases of heat stroke in the wild, sitting in a cold stream may help cool core temperatures. Burns can also cause significant water loss. Due to the loss of the skin barrier, the evaporation of fluid is much greater from the burned area. The larger the area of the burn, the more water is lost. A burn can also increase the risk of secondary infection due to the loss of the protective skin barrier. Even in a hospital setting, someone with a severe burn (third degree) over greater than 40 percent of their body can have a 40 percent chance of mortality.
In a survival situation, honey would be a good makeshift barrier for a burn, serving as a barrier as well as providing some antimicrobial coverage. Lastly, in a prolonged survival setting, the ability to maintain nutrition decreases, as does the amount of protein stored in your body. As the protein levels drop, it becomes more difficult to keep fluids in the vascular space and can lead to hypovolemia (a decreased volume of circulating blood in the body).
This is when the heart fails to function efficiently. When the heart weakens acutely because of a heart attack, there’s less muscle available to do work. Sometimes the cardiac muscle becomes weak over time due to heart failure, and no longer can meet the demands of the body. These situations decrease the heart’s ability to pump blood with each contraction and thus decrease stroke volume. Another reason the pump cannot meet demand is if the heart rate is too slow. As the heart rate drops, the heart muscle has to contract harder to push the volume of blood out to maintain cardiac output. Conversely, if the heart rate is too fast (over 200), the heart doesn’t have enough time to fill with blood between contractions, and the stroke volume decreases.
Mortality for cardiogenic shock in the hospital is around 50 percent. Normally, aspirin is given at the onset of a heart attack; however, if there’s no aspirin, natural salicylates would include willow bark, blackberries or red raspberries, cayenne pepper, and almonds. Several days rest would also be important for the patient. Using a drug to increase heart rate wouldn’t be wise. It’s likely a heart attack affected the pacemaker area of the heart, and putting chemical stress on the heart could further expand the area of heart muscle involved.

While external bleeding may not be present after bodily trauma, internal bleeding can often lead to the onset of shock.
This occurs when compression of the heart prevents it from filling with blood. This decreases the stroke volume, because the heart cannot generate enough force to contract. Examples of this would include tension pneumothorax and pericardial tamponade. In a tension pneumothorax, air leaks from a hole in the lung into the space between the lung and the chest wall. If the air cannot escape, then pressure builds within the space and creates the “tension.” The increased pressure in the chest doesn’t allow the heart to fill, and blood pressure falls. The neck veins (jugulars) become distended, and the trachea may even deviate away from the side of injury. The lifesaving measure is to use a decompression needle to allow the air to escape and decrease the tension. The decompression procedure is much more risky in a non-hospital setting.
Pericardial tamponade occurs when fluid builds up within the pericardial sac surrounding the heart. When this fluid accumulates (from trauma, infection, inflammation, or cancer), it prevents the heart from filling with blood due to the constriction and increased pressure in the pericardial space. This can also cause a decrease in blood pressure or signs of congestive heart failure. Natural diuretics like grapes, garlic, onions, dandelion, and green tea could be used to help with congestive heart failure; however, the likelihood that these will be strong enough or act quickly enough to overcome the effects of pericardial tamponade is very low.
Shock is a devastating process that has about a 50-percent mortality rate in the hospital setting. In a survival situation with no immediate help, the chances of survival are poor. The best chance of survival is to prepare for causes that can be reversed (e.g. anaphylaxis, hypovolemia, and hemorrhage). Ensure adequate hygiene to prevent even the simplest of scratches from leading to sepsis. Natural plants are helpful for many situations, but aren’t likely to be potent enough or work fast enough to make a difference in the case of shock. And if you haven’t already, take a basic first-aid course and continue with more advanced education so you’re better prepared to handle an emergency.
David Miller, DO, FACOI, is an internist in private practice. Diagnosed with Type 1 diabetes in 1990, he has a unique perspective on patient care and disease management. Experiences away from the office include being a fight doctor for regional MMA bouts and a team physician for a Division I university in west central Illinois. Dr. Miller is an instructor for the Civilian Crisis Response Team (medical section) based out of Indianapolis.
Don’t miss essential survival insights—sign up for Recoil Offgrid's free newsletter today!
Read articles from the next issue of Recoil Offgrid: Issue 31
Read articles from the previous issue of Recoil Offgrid: Issue 29
Check out our other publications on the web: Recoil | Gun Digest | Blade | RecoilTV | RECOILtv (YouTube)
Editor's Note: This article has been modified from its original version for the web.
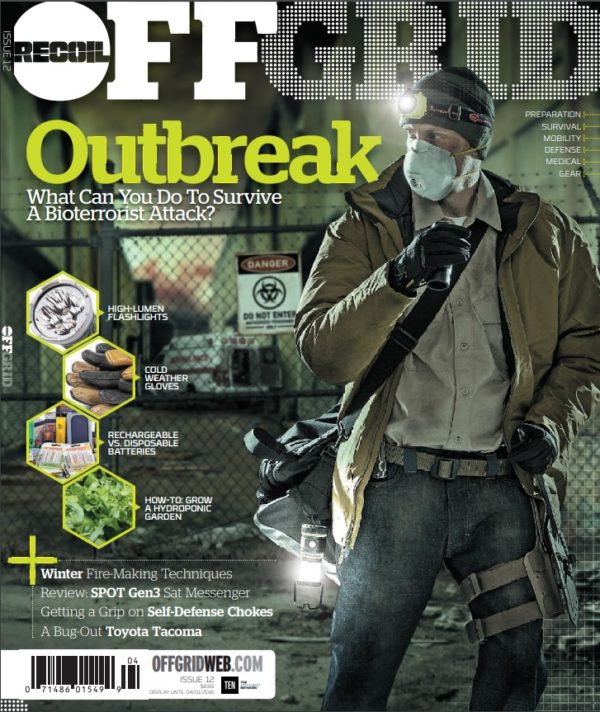
 STAY SAFE: Download a Free copy of the OFFGRID Outbreak Issue
STAY SAFE: Download a Free copy of the OFFGRID Outbreak Issue
No Comments